Urinary incontinence is the name given to the situation where a person cannot hold their urine, either unintentionally or consciously. In order to understand the type of urinary incontinence, it is useful to understand how we can control our urine and how the urination process is controlled.
The urine filtered from the right and left kidneys is brought to the bladder through channels called ureters. The bladder is a hollow organ and as urine fills, it transmits to the brain the increase in pressure inside it through receptors on the cells lining it. When approximately 400-500 ml of urine accumulates in the bladder, messages are transmitted from the bladder to the brain via nerves that the bladder is full and needs to be emptied. If the environment is not suitable at the time of this message, i.e. if there is no toilet for urination, the brain sends messages to the bladder and instructs the bladder to relax more and increase its capacity, and to tighten the outlet to prevent urine leakage. When the conditions become suitable, i.e. when the person reaches the place and conditions where he can urinate, the brain sends another message to the bladder and commands the muscles of the bladder to contract, the part called the urethra that drains urine to the outside, and the muscles surrounding this part to relax. In this way, the bladder contracts and increases the pressure inside, allowing urine to flow outward, similar to emptying the liquid inside a balloon, and this command is terminated when the urine runs out from the bladder.
As can be understood from the above, emptying the bladder, that is, urinating, is a complex procedure. Initially, after the bladder is filled with urine, a command is sent to the brain, the brain perceives this command and sends the command to the bladder to empty or not to empty, the nerves that send the command from the bladder to the brain must be healthy, and the nerves that send the commands from the brain to the bladder must also be intact. Any damage to the nerves that mediate the command from the bladder to the brain that the bladder is full or the command from the brain to the bladder to empty or not to empty would disrupt this process and cause uncontrolled urine leakage.
There are some obstructive sphincter mechanisms that contribute to the storage of urine in the bladder and prevent it from flowing out involuntarily. The urethra, a tube-shaped organ that drains urine from the bladder to the outside of the body, contains some muscle structures within itself. By contracting these muscles, it closes the inside of the channel and prevents involuntary urine leakage. In addition to the structure called the urethra, some muscles called the pelvic floor muscles squeeze the urethra from the outside, narrowing the inner space of the urethra and helping to prevent involuntary urine leakage from there.
Problems that arise in any of the mechanisms described above will present as involuntary urinary incontinence. As can be understood from above described mechanisms, involuntary urinary incontinence includes more than one type.
Stress urinary incontinence is the involuntary loss of urine in situations where intra-abdominal pressure increases, such as coughing, sneezing, laughing, or lifting heavy objects. Normally, in the situations listed above that increase intra-abdominal pressure, the muscles at the exit of the bladder and the sphincters of the urethra come into play to prevent the involuntary leakage of urine. The weakness in the muscles mentioned above, called the pelvic floor muscles, surgical procedures in this area, obesity, old age, smoking, being overweight, etc. causes the pelvic floor to become weaker. In these situations if intra-abdominal pressure increases, it cannot provide enough resistance and allows the urine to exit involuntarily.
Stress urinary incontinence, i.e. leakage of urine during coughing, sneezing and laughing, is both a health problem and a serious social problem. In such cases, patients with urinary incontinence often hide their complaints, constantly use diapers, have hesitations about leaving their homes, limit their social activities and worry that a new, bad period has begun for them. Since the issue of urinary incontinence is considered to be private to some extent and is perceived as a situation to be ashamed of, it is often not discussed with doctors or family members, and no effort is made to seek a solution. Most of the time, we, gynecologists, become aware of the existence of urinary incontinence not as a complaint of the patients themselves, but as a result of our questioning them about their complaints.
In individuals who are diagnosed with urinary incontinence during coughing, sneezing, laughing, or heavy lifting, it may be determined that the bladder sags slightly during the gynecological examination. If a cotton catheter is sent from the urethra to the bladder during the gynecological examination and the intra-abdominal pressure is increased by straining or coughing while the catheter is in the urethra, if the catheter moves upwards by more than 30 degrees, it is thought that the neck of the bladder moves with coughing and this movement is the cause of involuntary urinary incontinence. If the patient is strained or coughed during the gynecological examination while the bladder is full, it can be observed that urine comes out of the urethra involuntarily, and that the urinary incontinence is in the form of stress urinary incontinence. Since urinary tract infections contribute negatively to urinary incontinence, it will be necessary to carefully investigate whether there is an infection in the urinary tract during the evaluation of the patient, as well as whether there are other pathologies that may affect the bladder.
If the type of urinary incontinence is stress urinary incontinence and there is no other external pathology contributing to this condition, the treatment of this condition is usually surgery. The aim of surgical treatment is to perform support surgeries that prevent the neck of the bladder from sliding downwards when coughing, sneezing, laughing, in other words, when the pressure inside the abdomen increases. Thanks to support surgeries, the neck of the bladder will be prevented from sliding downwards when the abdominal pressure increases, and therefore the urinary incontinence will be treated. This is the expectation from surgeries. Many types of surgeries have been defined for this purpose.
Some of the surgeries are performed vaginally while some of them abdominally. In surgeries performed vaginally, the vagina is usually cut to reach the neck of the bladder, and supportive stitches or supportive patches are used to prevent the bladder from moving downwards. Surgeries performed vaginally with patches are generally successful. Since the surgeries are short-term and are performed vaginally, without entering the abdomen, less post-operative pain and similar negativities are encountered. However, one of the negative aspects of surgeries performed vaginally is that the problem is more likely to recur within 5-10 years after these surgeries, and also that problems called patch erosion occur in the vaginal mucosa due to the patches used during the surgery. In patch erosion, the patches used during the surgery melt the vagina in that area, the patch comes out of the vagina and becomes visible, and it becomes necessary to remove these patches. When planning the surgery, it would be appropriate to provide informative information about the higher risk of recurrence in surgeries performed vaginally and patch erosion.
One group of surgical methods used in the treatment of stress urinary incontinence is surgeries performed through the abdomen. These are also called abdominal surgeries. The purpose of these surgeries is to prevent the downward movement of the area at the exit of the bladder by hanging it to the places defined above in cases where intra-abdominal pressure increases such as coughing, sneezing and straining. The most commonly used surgical method for this purpose today is the method called ''Abdominal Burch''. During the surgery, the area at the exit of the bladder is pressed by the sutures passed through this area and the connective tissue called Cooper ligament at the upper parts of the pelvic bones is pressed by the stitches passed through this area, preventing this area from sliding downward in cases such as coughing, sneezing and straining. Abdominal Burch surgery can be performed both by opening the abdominal cavity, such as a cesarean section, or by entering this area with laparoscopy, that is, with the help of a camera, without opening the abdomen in this way. The success of Abdominal Burch surgeries is similar, independent of open or laparoscopic. Approximately 90-95% positive results are obtained in all surgeries. The advantage of laparoscopic surgeries over open surgeries is that the return to daily life is shorter after surgery. Patients can return to their routine daily activities a few days after surgery. Another important issue that patients should be informed about during surgery planning is that the success of the surgery is not 100% and that some problems may arise after surgery. Bleeding during surgery, infection after surgery, difficulty urinating after surgery and incomplete emptying of the bladder are the problems and complications that can be encountered in these surgeries. TOT (Transobturator Tape) and TVT (Transvaginal Tape) surgeries are also frequently performed surgeries for stress urinary incontinence through the vaginal route. The fact that these surgeries are performed vaginally and do not require entering the abdomen shortens the surgery time and increases surgical comfort. Unfortunately, the positive effects of the surgeries last for a shorter period, and the possibility that the patches used in the surgeries (especially the patches used for TOT surgery) cause erosion in the vagina and need to be removed reaches 10%, which causes us to prefer TOT and TVT surgeries less in our clinical practice.
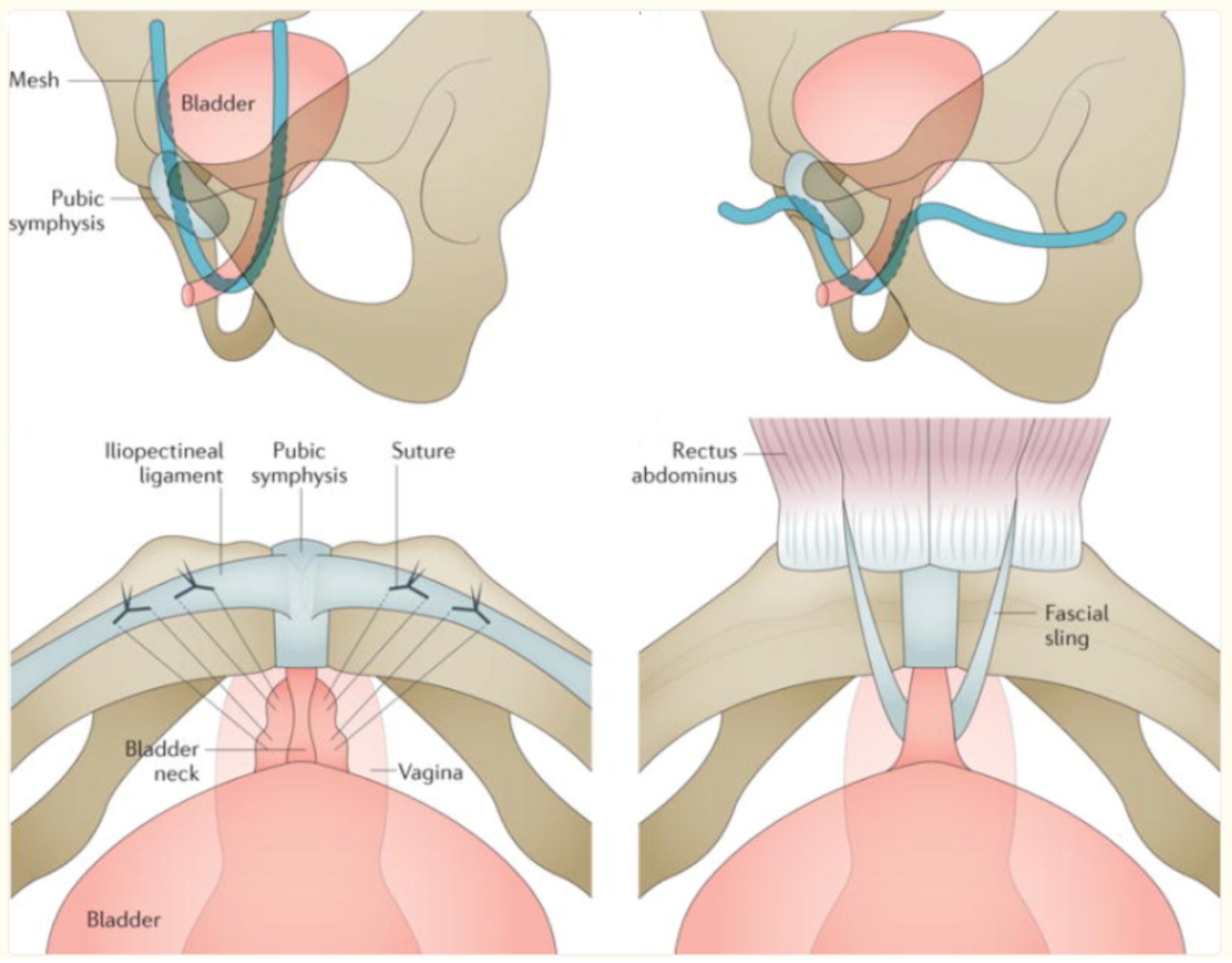
Some of the surgical methods applied for Stress Urinary Incontinence in women. Schematic. Image adapted from Aoki Y et al 2017.
Urgency urinary incontinence, that is, when the bladder is full and the urge to urinate occurs, urine leakage on the way to the toilet without being able to hold it in, is defined as urgency incontinence. Patients with urgency urinary incontinence usually do not want to leave the house. When they go to a shopping mall or another environment, they first check where the toilets are, try to drink as little liquid as possible, and try to plan their lives in a way that is structured between urinary incontinence and the toilet.
The exact cause of urgency incontinence has not been determined. However, as explained above, it is thought that the processes related to suppressing urination under unsuitable conditions after the brain is informed that the bladder is full do not work properly. The problem may occur with the contributions of the bladder nerves, the bladder muscles and the pelvic floor muscles that help hold urine outside. Another common underlying cause is the involuntary contraction of the bladder muscles, called overactive bladder, spontaneously and before the bladder is full. If no additional cause, treatment is usually to increase the capacity of the bladder with medical treatment to suppress uncontrolled contractions and Kegel exercises to strengthen the pelvic floor muscles, lose weight, quit smoking, etc.
In addition to those above described, there are also cases such as Mixed Urinary Incontinence, where more than one type of urinary incontinence coexists. Sometimes, understanding the type of urinary incontinence and the underlying problem may not be as easy as described above. For this purpose, more advanced examinations, tests such as urodynamic tests, and even approaches that require more than one department to work together may be needed.
The thing that is recommended to be kept in mind about urinary incontinence in women is that this condition is not something to be shameful or hidden. If you go to a doctor and explain your complaints, and if the necessary examinations and tests are done, in most cases, urination can be controlled by using medication, surgery, exercise or a combination of these.